Transforming care, rewarding excellence Providers grow with the ACO REACH model
Put patients first while earning the compensation you deserve. With Medicare’s ACO REACH model, providers can deliver exceptional care, improve access, and achieve better outcomes-all while benefiting from a financial model that values quality and equity.
What ACO REACH can do for your practice and your patients
The ACO REACH model empowers providers with financial stability, operational support, and tools to make meaningful changes for patients.
-
Minimum risk, maximum reward
Earn above Medicare’s physician fee schedule with no downside risk.
-
Flexible & Scalable
Solutions designed to adapt to diverse practice types and operational workflows.
-
Shared Savings Rewards
Retain more of the savings generated through patient-centered care.
-
Financial transparency
Monthly clinical and financial performance reports specific to your patient population.
-
Care Coordination Support
Extend your practice with ilumed’s team of RN Care Coaches, Social Workers and Patient Advocates.
-
Value-Based Care Technologies
Access to best-in-class technology platforms to simplify patient risk stratification and support services.
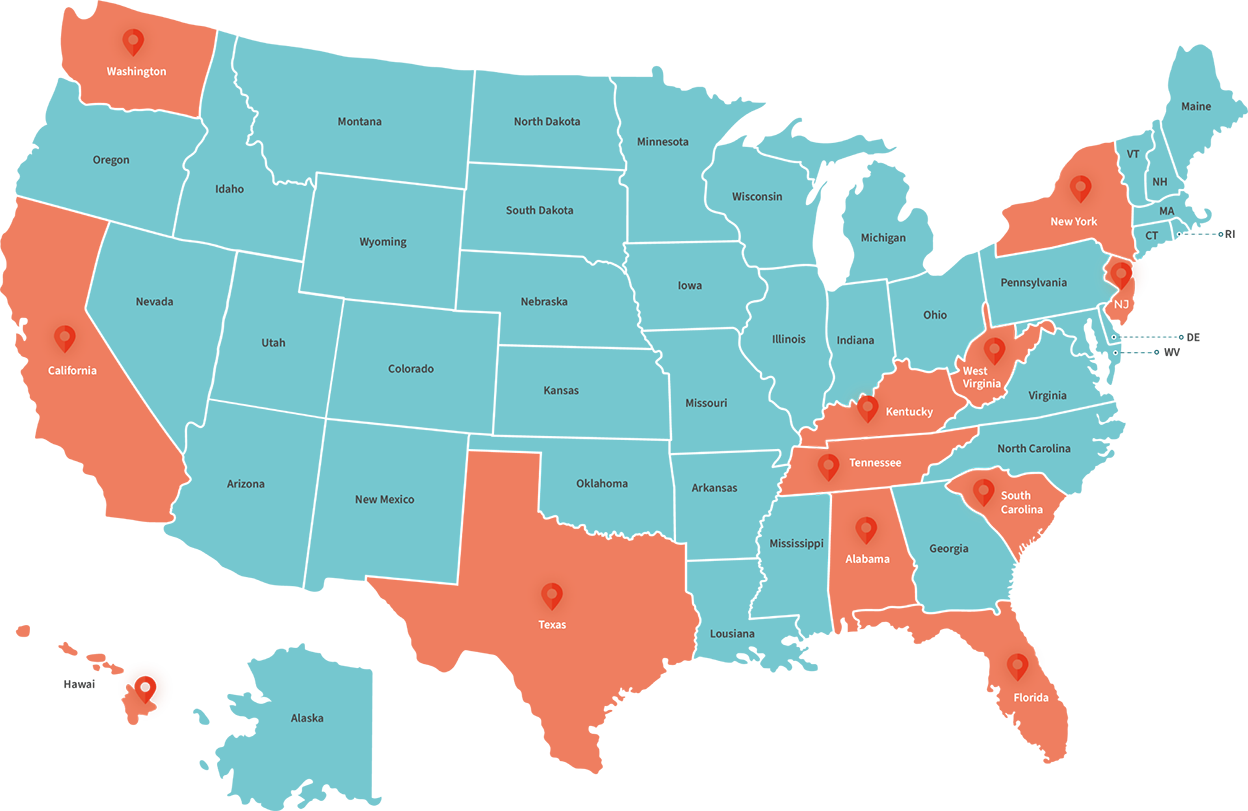
ilumed's reach, your impact
-
12
states
-
700+
primary care providers
-
6.3%
gross savings rate
Provider-focused thought leadership
Learn from ilumed’s executive team how to enhance your clinical and administrative operations while fostering a culture of compassionate, patient-first care.
ilumed: Your Partner in practice transformation
With ilumed by your side, you’ll have the tools, expertise, and support to thrive in value-based care.
-
Operations transformation
Streamline workflows and improve your financial position. Deliver better care with scalable, data-driven systems.
-
Shared Surplus Opportunity
-

Harness analytic insights to support providers in managing their panel of Medicare patients.
-

Clinical programs purpose-built for the needs of Medicare patients.
-
-
Advanced technology
Gain actionable insights with population health analytics. Improve visibility to patient disease burden at the point of care.
-
Enhanced visibility to a patient's chronic conditions and treatments
-

Insights to prioritize the patients with significant unmet needs.
-

Training and support for efficient deployment.
-
-
White-glove service
Providing personalized support for high needs patients, both clinically and socially.
-

Appointment and transportation scheduling
-

Assistance in removing barriers to care
-
Team-based case and disease management
-

